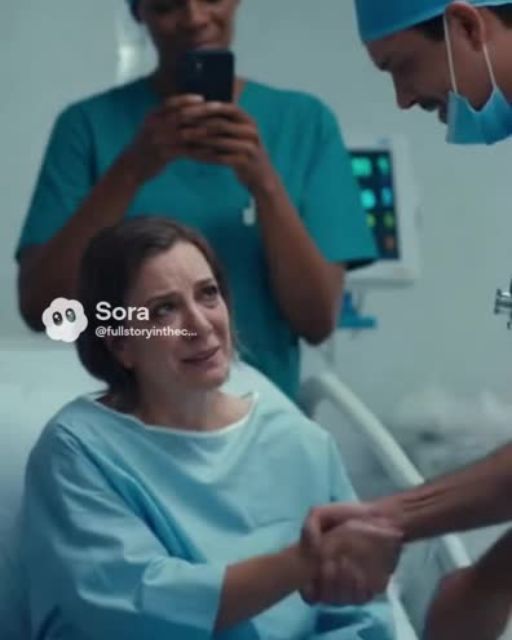
They had already wheeled my mother into pre-op when the nurse came running in, pale and panicked.
“I’m so sorry… the doctor says he won’t proceed until your payment clears.”
I blinked. “What payment? We already paid our portion. The insurance—”
“He said it’s flagged as unpaid. He’s refusing to operate.”
Refusing to operate. On a 67-year-old woman with a fractured hip and internal bleeding.
I tried to talk to him—Dr. Halvorsen. Cold, robotic, and too busy checking his watch to look me in the eye.
“Hospital policy,” he shrugged. “You’re welcome to reschedule once it’s sorted.”
I stood in the hallway shaking, staring at a man who was choosing money over a human life.
But he had no idea who was standing behind me.
A man in blue scrubs. Arms folded. Watching everything.
Dr. Naved, the head of trauma surgery—and my late father’s closest friend.
He stepped forward, looked Halvorsen dead in the eye, and said, “I’ll take it from here.”
Within minutes, my mom was in the OR—with a new team, a new doctor, and no delay.
I thought that was the end of it—until the video surfaced.
One of the nurses had caught the whole exchange on her phone. Posted it anonymously. The hashtags exploded.
By morning, it had 3.2 million views and counting.
But here’s what really did him in:
A former patient came forward with her own story—almost identical. Same doctor. Same stunt. But her outcome was… different.
Her name was Lillian, a retired librarian from two towns over. She said she had gone in for gallbladder surgery last year. The anesthesiologist had already placed her IV when Halvorsen walked in demanding payment confirmation.
She said she didn’t have her phone or paperwork with her, and no one from her family had arrived yet.
He postponed the surgery for seventy-two hours.
By the time they rescheduled, her gallbladder had ruptured. She went septic.
She survived, barely, but her kidneys never recovered. She’s been on dialysis since.
She said she complained, begged the hospital to investigate, tried to get someone—anyone—to take her seriously.
She said they ignored her.
Until the video of my mom’s situation surfaced.
The more people watched, the more they started digging. Turns out Lillian wasn’t alone. The pattern was there—quiet, buried under paperwork, brushed aside by administrators who didn’t want the trouble.
Three more families came forward. All the same story: Halvorsen refusing treatment until payment cleared. Some patients suffered permanent consequences. One didn’t make it.
But none of this was public. Not yet.
That changed when a woman named Carla posted a long thread with screenshots, medical records, and emails she’d sent the hospital. She had lost her husband after his appendix burst while Halvorsen refused to operate for “insurance verification.”
The thread went viral within hours.
By dinner time, every major news outlet was calling the hospital.
But the biggest twist? The part no one saw coming?
It happened two days later.
The hospital held a press conference to address the growing outrage. People were expecting an apology, maybe a suspension, maybe some words about “reviewing policies.”
But the board chair stepped forward and announced something shocking.
“Effective immediately, Dr. Martin Halvorsen is placed on administrative leave pending a full federal investigation.”
Federal.
People gasped.
But then the chair turned to a second page of her statement—and her voice shifted.
“We would also like to address claims that hospital administration was unaware of any misconduct. That is inaccurate. Multiple complaints were received over the past three years.”
I felt my stomach flip.
She cleared her throat.
“These complaints were dismissed not by lack of evidence, but by deliberate interference from internal leadership. In light of recent revelations, we have discovered that Dr. Halvorsen has been receiving undisclosed payments through a third-party billing contractor. This contractor has been…” She paused. “…terminated.”
The reporters erupted.
I froze.
Undisclosed payments?
Then it clicked.
He was refusing surgeries so that certain “urgent billing clearances” needed to be processed through one specific contractor—one that kicked money back to him for every case delayed.
Every hour a surgery was postponed, the contractor charged “priority processing fees.”
Fees that patients didn’t know were optional.
Fees that insurance companies often denied, leaving patients stuck with surprise bills.
Fees that somehow always led back to Halvorsen.
It wasn’t just greed.
It was a scheme.
And the worst part?
It had been happening for years.
That night, the story blew up even more. Hospital protests formed within hours. Former nurses, techs, and even a few residents came forward, saying they had always felt something was “off” with him.
But no one expected the next twist—not even me.
It came from my father’s old colleague, Dr. Naved.
He knocked on my door at eight in the evening, exhausted but determined.
“I need to tell you something,” he said.
We sat at my kitchen table, the news playing quietly in the background. My mom was recovering upstairs, still groggy but stable.
He folded his hands.
“I knew Halvorsen was difficult,” he said. “I knew he cut corners, pressured residents, made comments about patients wasting his time. But I didn’t know the extent of this. I should’ve looked deeper.”
I shook my head. “This isn’t on you.”
But he wasn’t finished.
“There’s a woman you should talk to,” he said. “She used to work billing for the hospital. She was fired after raising concerns.”
“Fired for what?”
“For reporting missing documents, inconsistencies, signatures that didn’t match.”
I frowned. “Signatures?”
He nodded.
“We think Halvorsen forged approvals. Maybe even patient consents. Enough to stall surgeries in a way that looked legal on paper.”
My jaw dropped.
“And she tried to tell someone. She tried repeatedly. The contractor got her dismissed.”
“Do you know where she is now?” I asked.
He nodded again.
“She reached out to the board after the video. She’s willing to talk to you.”
The next day, I met her in a coffee shop near the courthouse. Her name was Melinda. Early 40s, tired eyes, looked like someone who’d spent years shouting into a void.
She told me everything.
And I mean everything.
How she noticed certain charts being pulled for “payment verification” even when insurance had already confirmed coverage.
How surgeries under Halvorsen were statistically more likely to be delayed for “administrative review.”
How she reported discrepancies and got written warnings in return.
How her final straw was a case involving a teenage boy whose appendix was ready to burst. She begged administration to override the delay. The contractor declined. Halvorsen refused responsibility.
The boy survived—but only after being rushed into emergency surgery by another doctor who happened to be passing through.
Melinda said she was fired the next morning.
She took a sip of her coffee and whispered, “I thought maybe I was crazy. That maybe I was overreacting. But after seeing your mom’s video… I knew I wasn’t.”
I sat there stunned, trying to process everything.
But the biggest twist was still coming.
A week later, during the federal inquiry, investigators uncovered something hidden in the billing contractor’s software.
An automated flag system.
You know what triggers it?
Patients over fifty-five.
Patients with chronic conditions.
Patients with government insurance.
Patients who looked like “high-risk cases” for delayed payments.
In other words—
the most vulnerable people.
Their cases weren’t randomly delayed.
They were targeted.
It wasn’t just Halvorsen’s greed—it was a full-blown predatory system that counted on sick, scared patients not having the ability or time to fight back.
The outrage reached a breaking point. The contractor’s CEO resigned. Hospital leadership was overhauled. Lawsuits piled up.
But what happened to Halvorsen shocked everyone.
I expected him to lawyer up, deny everything, maybe hide behind some technical medical jargon.
Instead, the day the investigation findings went public, he disappeared.
Vanished.
Didn’t show up to work.
Didn’t answer calls.
Didn’t appear in court.
People speculated he fled the country.
Others thought he was hiding with family.
Turns out the truth was much simpler—and much sadder.
He was found two towns away, staying in a cheap motel, eating vending machine snacks, and pacing in circles like a man who knew the world outside was closing in.
When police found him, they said he kept muttering the same thing over and over:
“I didn’t mean for anyone to get hurt.”
He didn’t fight.
Didn’t argue.
Didn’t resist.
He just… surrendered.
His medical license was revoked.
He faced multiple charges.
His entire career collapsed in days.
But that wasn’t the ending people talked about.
No.
The ending everyone remembered—the one that felt like some kind of karmic balancing—came a month later.
The hospital announced a new policy.
Every delayed case would now undergo an independent review by two separate physicians.
Payment disputes could no longer delay life-saving procedures.
Billing contractors would be monitored by third-party auditors.
But that wasn’t even the best part.
A new foundation was created, named after Lillian—the retired librarian who first spoke out.
It was called The Lillian Patient Advocacy Fund.
Its purpose?
To help vulnerable patients cover emergency medical costs, fight unjust bills, and get legal support when doctors or hospitals tried to pull the same stunt.
Guess who spearheaded the fund?
Dr. Naved.
And my mom.
She insisted on being part of it the moment she heard about it. She said if she survived everything she’d been through, the least she could do was help someone else.
At the launch event, she stood at the podium, leaning on her cane, wearing her favorite blue sweater.
She said, “I was scared that day. I thought I was going to die because someone decided my life wasn’t worth the paperwork. I don’t ever want another family to feel that.”
The room went silent. Cameras flashed. Reporters scribbled furiously.
Then she added, “We can’t change what happened. But we can make sure it doesn’t happen again.”
People applauded for almost a full minute.
But the moment that hit me hardest came after the event, when Melinda—the billing employee who had been fired—walked up to my mom.
She said, “Thank you. You spoke for all of us.”
My mom hugged her and whispered, “Thank you for speaking first.”
In the end, the story did more than take down a bad doctor.
It exposed a broken system.
It protected future patients.
It gave voices back to the people who were ignored.
And it reminded me of something my father used to say:
“Courage doesn’t always roar. Sometimes it’s a shaky nurse with a phone, a fired employee with documents, or a scared son who steps forward anyway.”
Today, my mom is walking again.
She gardens. She bakes. She laughs more than she cries.
And every time someone recognizes her from the viral video, she smiles and says, “Good. Keep talking about it.”
Because the more people know,
the harder it is for injustice to hide.
If there’s one thing this whole mess taught me, it’s this:
Sometimes the worst moment of your life becomes the spark that protects hundreds of others.
And sometimes karma doesn’t come like lightning.
Sometimes it arrives slowly—piece by piece—through truth, courage, and people who refuse to stay silent.
If you found this story meaningful, share it with someone who needs to hear it. And don’t forget to hit like—it helps more people find it.